Robert Bradley, 59, founder of a website for dog owners in Los Angeles, is committed to getting every COVID-19 vaccine booster he’s eligible for. His father died from COVID-19-related complications early in the pandemic, and he received the initial vaccine series as soon as it was offered. He got his first booster shot in January 2022.
“I know that the likelihood of dying is very low, if vaccinated,” Bradley says. “But I’m wary of the long-term effects of the virus.”
The only question now is when to get his recommended second booster.
“I keep hearing that I should get another one now, but I also keep hearing that the newer, more targeted booster is coming as early as September,” Bradley says. “I was traveling during the end of August and would have liked the most protection possible, but getting boosted then would have delayed my getting the updated booster until at least December.”
For better or worse, Bradley ultimately decided to wait.
“I’m going to depend on the three shots I’ve received already, along with masking and commonsense behavior, with the hope that the new booster is available sooner than later,” he says.
Like Bradley, many other people over 50 are making similar calculations in anticipation of bivalent shots that help protect against both the omicron subvariants BA.4 and BA.5, as well as the original virus. The new boosters, manufactured by mRNA vaccine makers Pfizer and Moderna, are expected to be released shortly, hopefully protecting Americans from potential surges of the rapidly evolving virus in the fall and winter.
Other vaccinated people have tired of the whole discussion and just want life to return to “normal.”
“Some people are saying, ‘I've received my initial series and I got my first booster. You’re asking for too much,’” says Zanthia Wiley, MD, assistant professor of infectious diseases at Emory University in Atlanta. “I tell them, ‘All of us are ready for this pandemic to be over and one of the way to get there is by as many as possible of us who are eligible for booster vaccines to receive them.’”
Booster basics
Boosters are designed to shore up waning defenses against the COVID-19 virus, says Michelle Barron, MD, senior medical director of infection prevention and control for UCHealth in Aurora, CO.
“The point of vaccination is to train your immune system to recognize and kill what’s targeting it,” she says. “Like all things, over time, if you don't practice, it’s harder to fight off an enemy. Getting a booster is like going through basic training again so your immune system is ready to kill it again.”
The Centers for Disease Control and Prevention (CDC) recommends the primary series of COVID-19 vaccines for everyone ages 6 months and older and a COVID-19 booster for everyone ages 5 years and older. (There are specific recommendations for people who are immunocompromised.) Two booster shots are recommended for adults ages 50 and older and people 12 and older who are immunocompromised.
People should receive an mRNA booster shot (Pfizer or Moderna) at least five months after the final dose in the primary mRNA vaccine series and at least two months after the Johnson & Johnson vaccine. Those 50 and older should get a second mRNA booster at least four months after the first booster.
Although the effectiveness of the boosters doesn’t match that of the first COVID-19 vaccines against the original virus (which was upward of 95% for mRNA vaccines), they do help to maintain protection against hospitalization and severe disease, particularly with the second booster — and even against omicron variants.
According to a July study from the CDC, protection against severe disease from omicron variants BA.1 and BA.2/BA.2.12.1 was 68% after a first vaccine booster, declining to 52% after six months. But when a second booster was administered, effectiveness shot up to 80% within the first six months. (after six months are not available yet.) That significantly reduced hospitalizations and emergency department visits caused by the omicron variant, the research shows.
Stay on track
That’s why infectious disease doctors are urging patients to stay on schedule with boosters, regardless of their virus components, receiving them as soon as they are eligible.
“A lot of people, including many of my patients who are eligible, are asking, ‘Should I wait until September for the bivalent vaccine before I get my second booster?’” says Wiley. “My advice is, Don’t wait. Go ahead and get your vaccine, especially now as we’re heading into the fall and winter, where we will have more circulation of respiratory viruses. It's best to boost your immunity as early as possible.”
Not everyone needs convincing. Leah and Bill Ingram of Slippery Rock, PA, both 56, got their vaccines and two boosters soon after each was available in their community.
“Given our age, we both have memories of lining up to get the rubella vaccine, which came out in the early seventies,” Leah says. “We were raised with this notion that if there is a vaccine that can save your life, that can save other people’s lives, you get it.”
In spite of the vaccines and other precautions, Bill had a bout of COVID-19 in early August.
“He was pretty sick for about seventy-two hours but he healed at home with the help of Paxlovid,” Leah says. “I can’t imagine how bad the disease would have been for him if he hadn’t been vaxxed and boosted.”
Still, while Barron wants her patients up to date on COVID-19 vaccination, she doesn’t discourage them from taking their individual circumstances into account.
”I like people to feel empowered to make choices about their medical care,” she says. “But some of the messaging around vaccines is meant to be simple and broadly applicable to everyone, which can prevent people from having conversations like ‘Does this really apply to me?’ For example, some people work from home, don’t have kids, and aren’t out and about. So it might make more sense for them to wait and get a booster right before a trip or a wedding.”
Countering booster burnout
As time has gone on and precautions like mask mandates have lifted, some patients need persuading that the first or second booster shots are even necessary. Wiley reminds them that the reason to get booster shots is the same as it was for the primary vaccines — and just as pressing.
“Some of my patients and even family members say, ‘I’m healthy, I’m okay,’” she says. “What I always say is, even though you are healthy and have received your primary vaccine series, the people who you are around and spending time with — say, your grandmother who has diabetes or the person next to you in the grocery store — may not be.”
Patients are also declining boosters for other reasons.
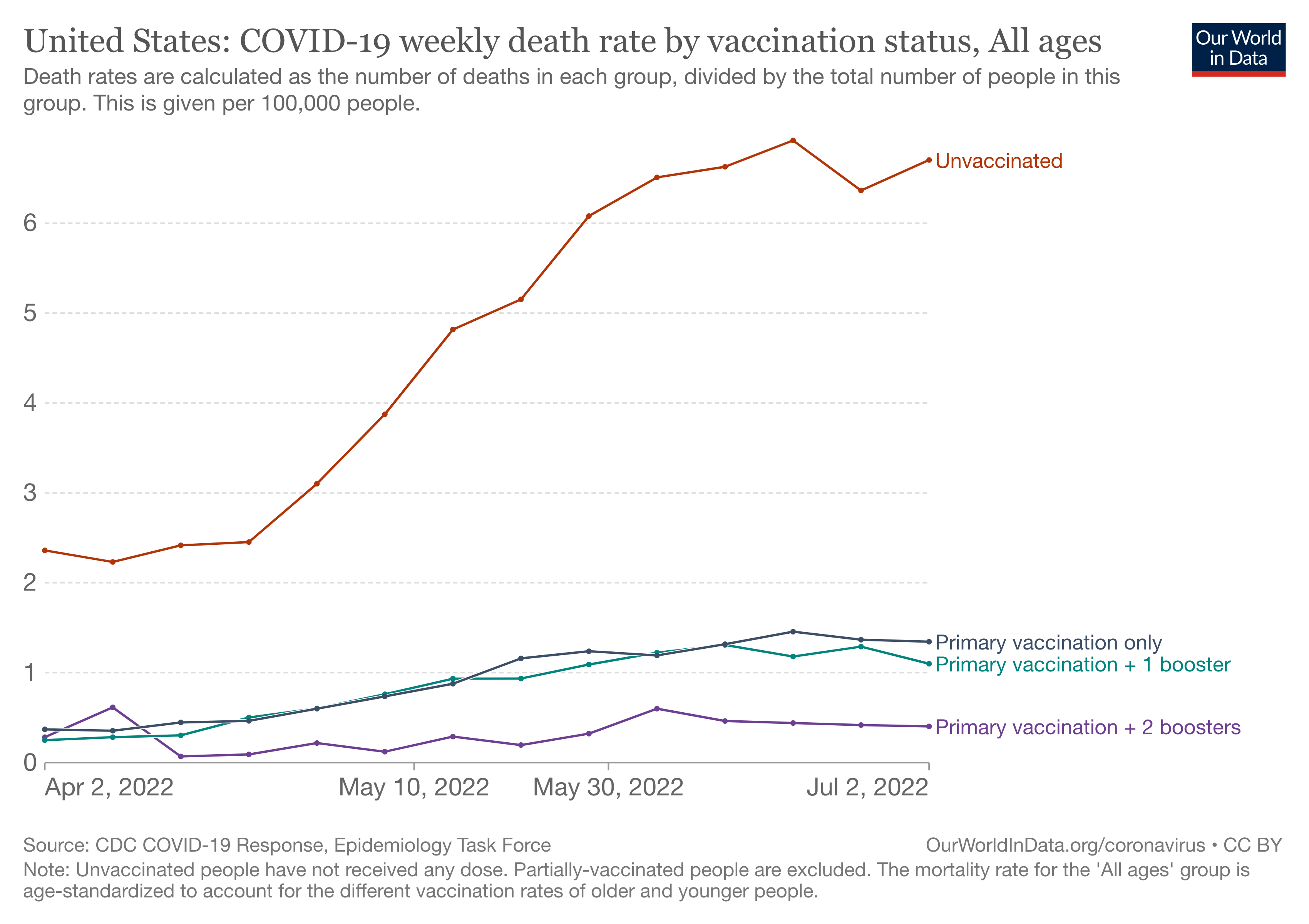
“They say, ‘I got vaccinated but I still got sick,’” Wiley says. “I try to remind them that that’s true of many vaccines, such as the flu shot. And I share that most of the people who are hospitalized and dying with COVID right now haven’t been vaccinated or boosted.”
It’s worth pointing out, too, that boosters may lessen the threat of long COVID-19 (or post-acute sequelae of SARS-CoV-2 infection), the sometimes debilitating symptoms that persist weeks or months after the illness, which affects around 10% of patients, Wiley says.
“Decreasing your likelihood of contracting COVID also decreases your likelihood of contracting long COVID,” she says. “It’s devastating to have a 40-year-old man with no prior medical problems not be able to work because of pain and fatigue due to long COVID.”
Although doctors and patients would like to move on from COVID-19, Barron says, it’s clear that the disease and the need for vaccines and boosters are here to stay, perhaps eventually leading to an annual vaccination.
“We have to start thinking of this as something that’s not going away,” she says. “And as we do with the flu, this is what we can do so that we don’t get sick.”
Zanthia Wiley and Michelle Barron also serve as members of the AAMC Multidisciplinary Advisory Committee that supports the AAMC-CDC Cooperative Agreement to build confidence in the COVID-19 vaccines.